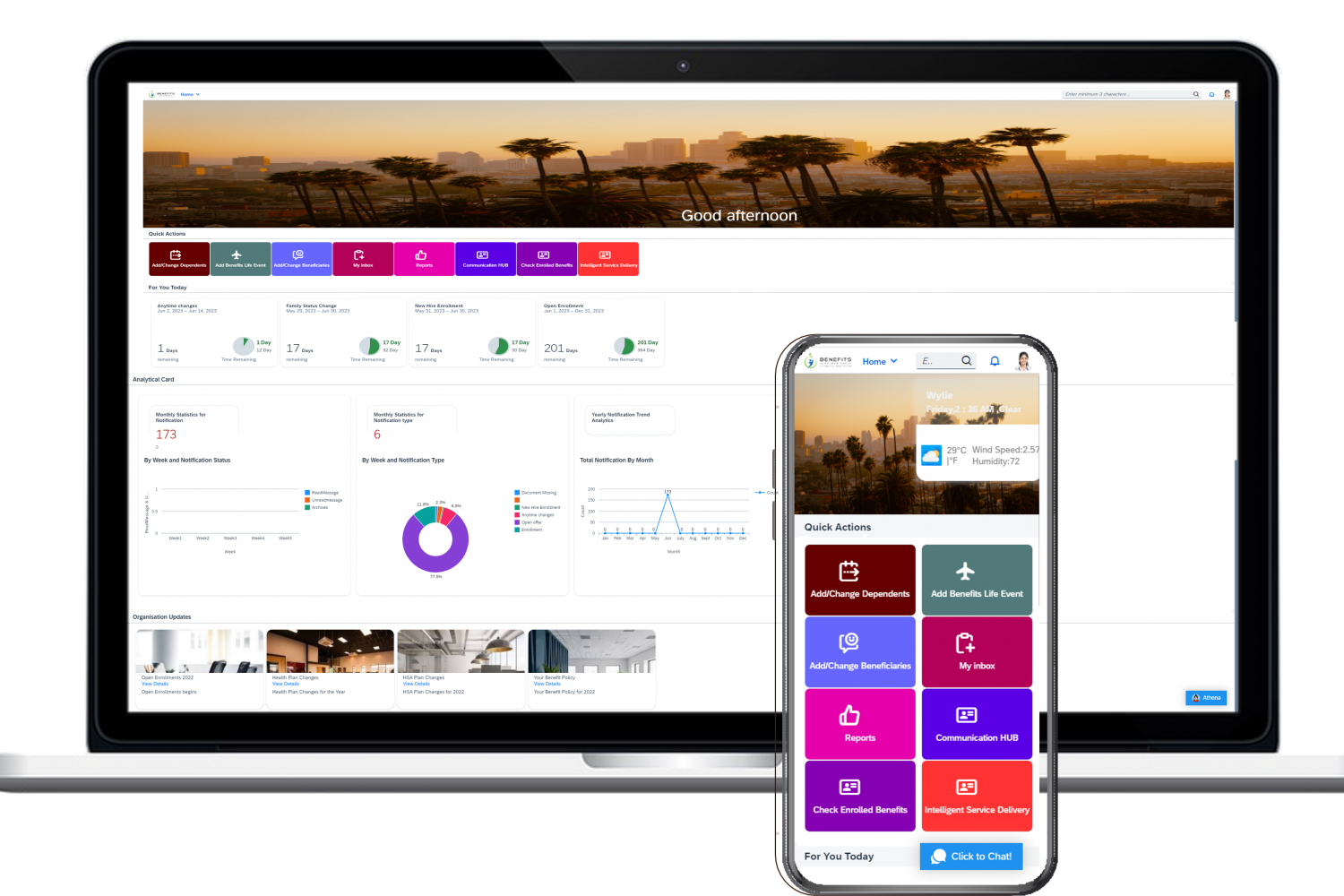
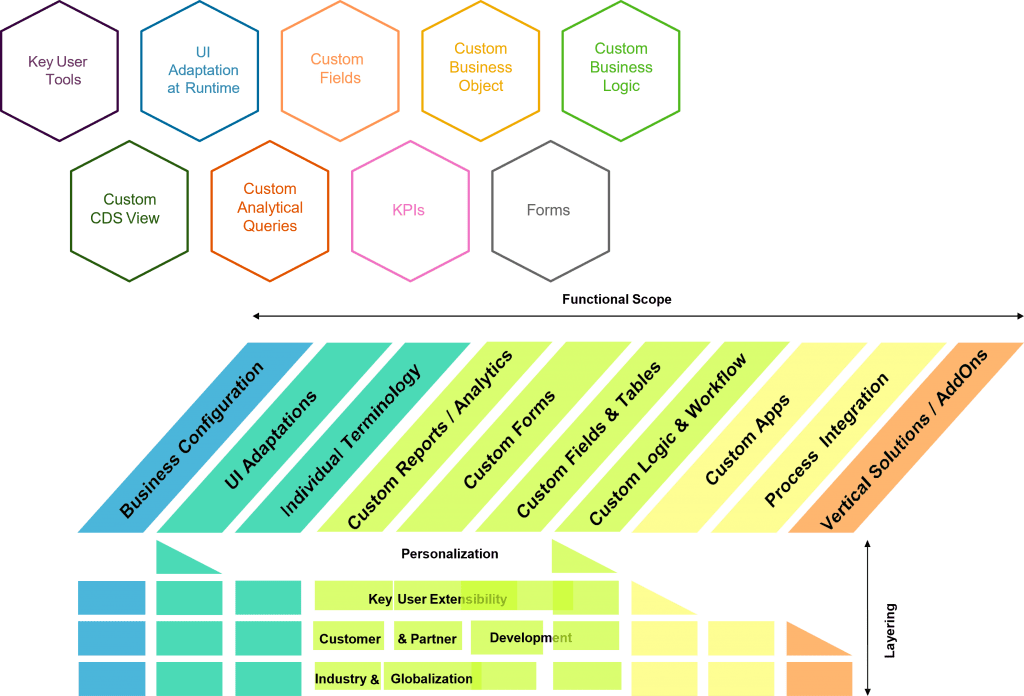
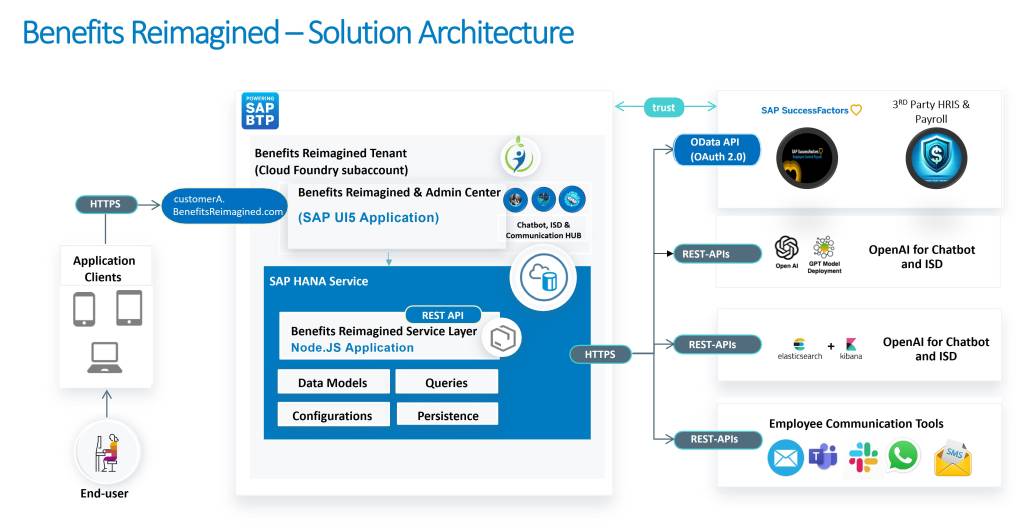
The only Benefits Application built entirely on SAP’s Business Technology Platform (BTP)
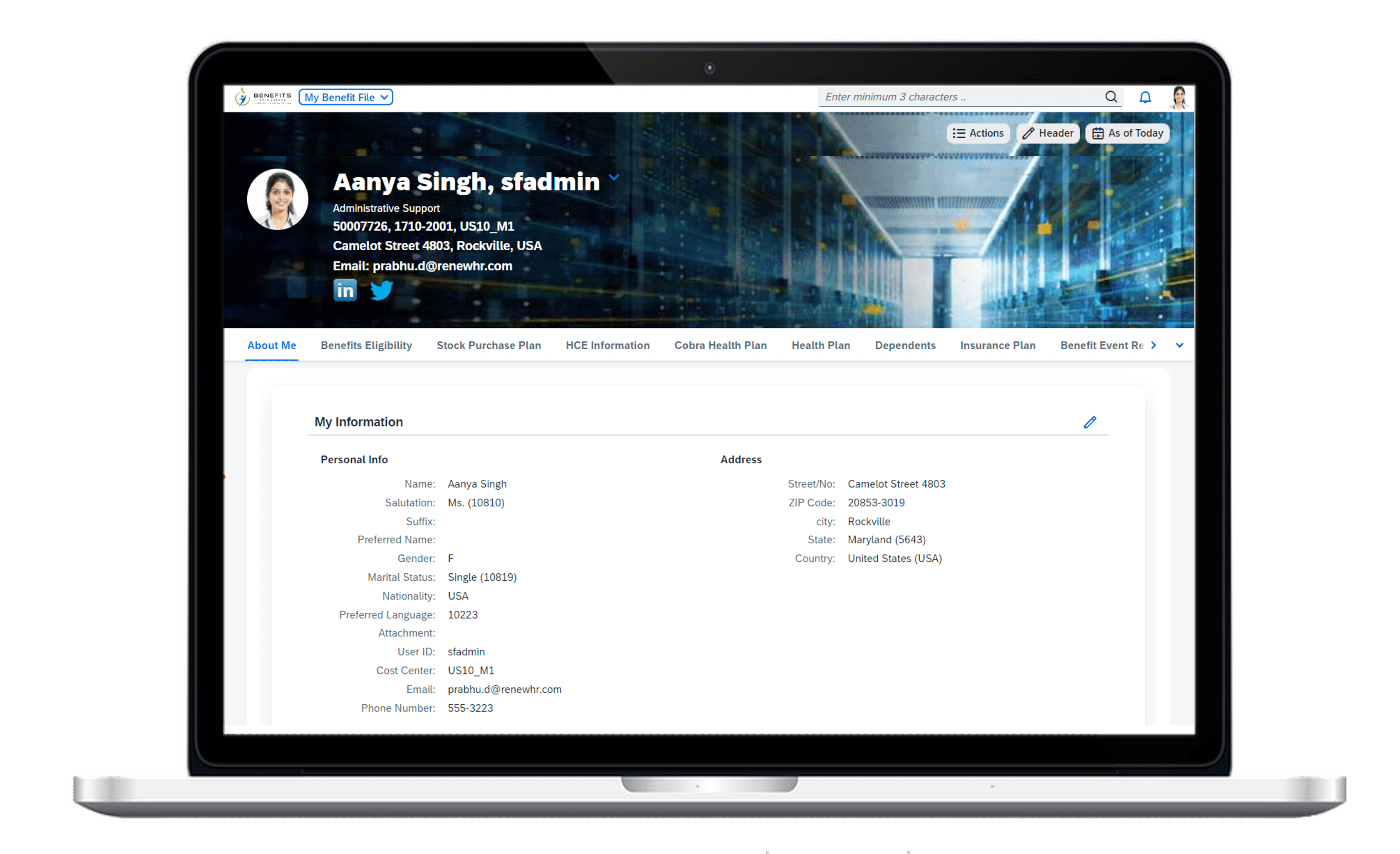
Full service, SSO enabled and embedded inside SuccessFactors with similar Look and Feel and navigation for Employee Central Customers.
All your Benefits at one place
- Benefits administration and management with flexible configuration and automation.
- Streamlined enrollment experience through the benefits and wellness dashboard.
- Enrollment and benefits management for employees.
- Dependents and beneficiaries’ management.
- Evidence of insurability management.
- Open enrollment and ERISA-compliant qualifying events.
- Health and wellness management, Savings, Insurance, HSA, FSA, Stock Purchase Plan, etc.
- Increased worker engagement and retention with flexible benefits programs.
- Each module, like Core Benefits, Communication HUB, and Intelligent Service Delivery (ISD), has a significant number of Reports and Analytics out of the box.
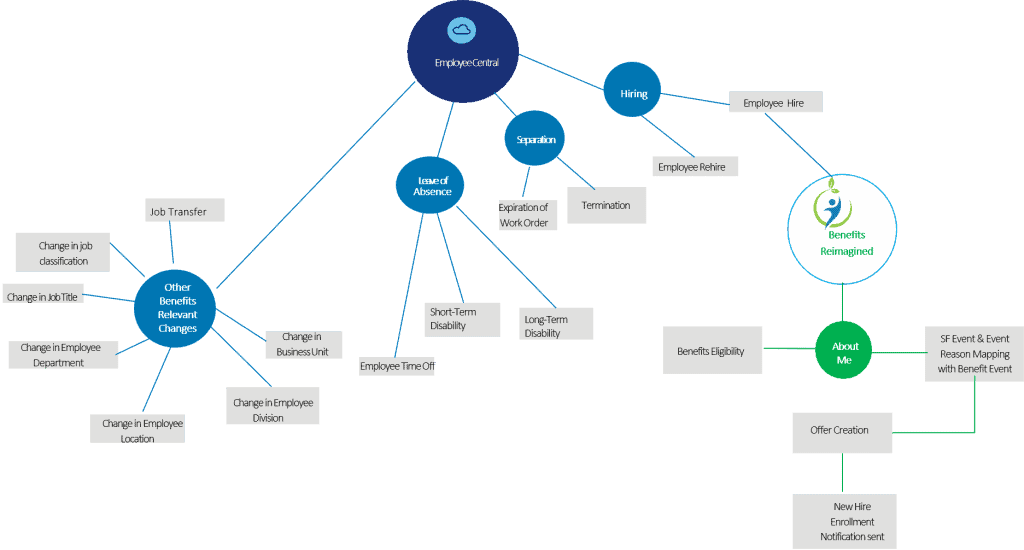
Embedded Benefits Application in SAP SuccessFactors Employee Central
- Benefits Reimagined is the Only full-service Benefits Application that is SSO enabled, Real-time, and can be completely embedded inside the SuccessFactors platform. The user experience is identical to existing SuccessFactors users, so no additional training is required for navigation.
- Unlike other 3rd party applications, the entire Benefits Reimagined’s employee benefits data resides within the SAP HANA Cloud environment eliminating data privacy and security concerns.
- All the features and functionalities of Benefits Reimagined are operational from within SuccessFactors.
- Reduces customer’s cost and time to implement integration between SuccessFactors Employee Central and Benefits Reimagined.
- Fast implementation of customer-specific integration between Success Factors Employee Central and Benefits Reimagined application based on templates and guides provided by Benefits Reimagined.
- The templates follow point-to-point integration, which makes them the perfect accelerator for most customers’ implementation.
- We leverage the SAP Business Technology Platform (BTP) without other integration tools.
You need a modern, sophisticated, and user-friendly UI that will help you increase participation and engagement.
Studies suggest Employee Benefits can help attract and retain employees in the current business environment.
Unified Core Vs. Apps using multiple APIs
Integrating AI and Elasticsearch into business applications is crucial for success in a data-driven environment, and a unified core codebase is critical. This unified approach enhances performance, simplifies development, provides a cohesive user experience, streamlines data management, and improves security.
In contrast, applications using multiple APIs face latency, complex maintenance, inconsistent user experiences, and increased security risks. Ultimately, choosing between a unified core and an API-driven architecture depends on the application’s specific needs and goals. Investing in a robust core is essential for effectively leveraging technology and fostering innovation and growth in the digital age.
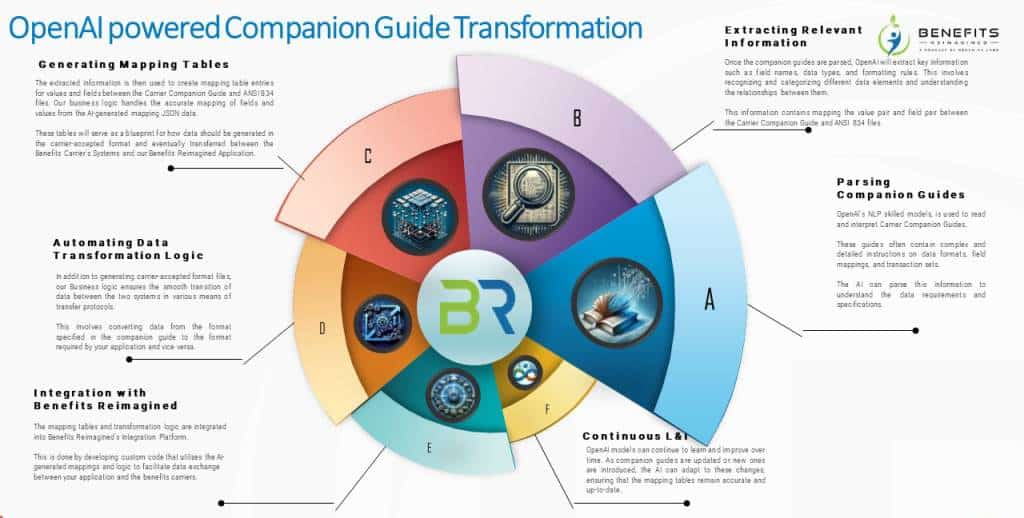
OpenAI-powered Carrier Integration
OpenAI’s NLP models efficiently interpret the complex information in Carrier Companion Guides, packed with detailed instructions on data formats, field mappings, and transaction sets. The models are designed to understand data requirements and specifications thoroughly.
Extracting Relevant Information
The AI processes these guides to capture details such as field names, data types, and formatting rules. It identifies and categorizes various data components and their interrelations, including mapping values and fields between the Carrier Companion Guide and ANSI 834 files.
Generating Mapping Tables
OpenAI generates mapping tables from the extracted data that align values and fields between the Carrier Companion Guide and ANSI 834 files, ensuring accurate mappings through our business logic.
Automating Data Transformation Logic
Our system creates carrier-accepted format files and facilitates the smooth transfer of data between systems using various protocols, converting data as the companion guides require.
Integration with Benefits Reimagined
The mapping tables and transformation logic are integrated into the Benefits Reimagined Integration Platform, using custom code based on the AI-generated mappings to support efficient data exchanges.
Continuous L&I
OpenAI models continuously learn and improve, adapting to updates or new guides to maintain up-to-date and accurate mapping tables and ensure data integrity and accuracy in transformations.
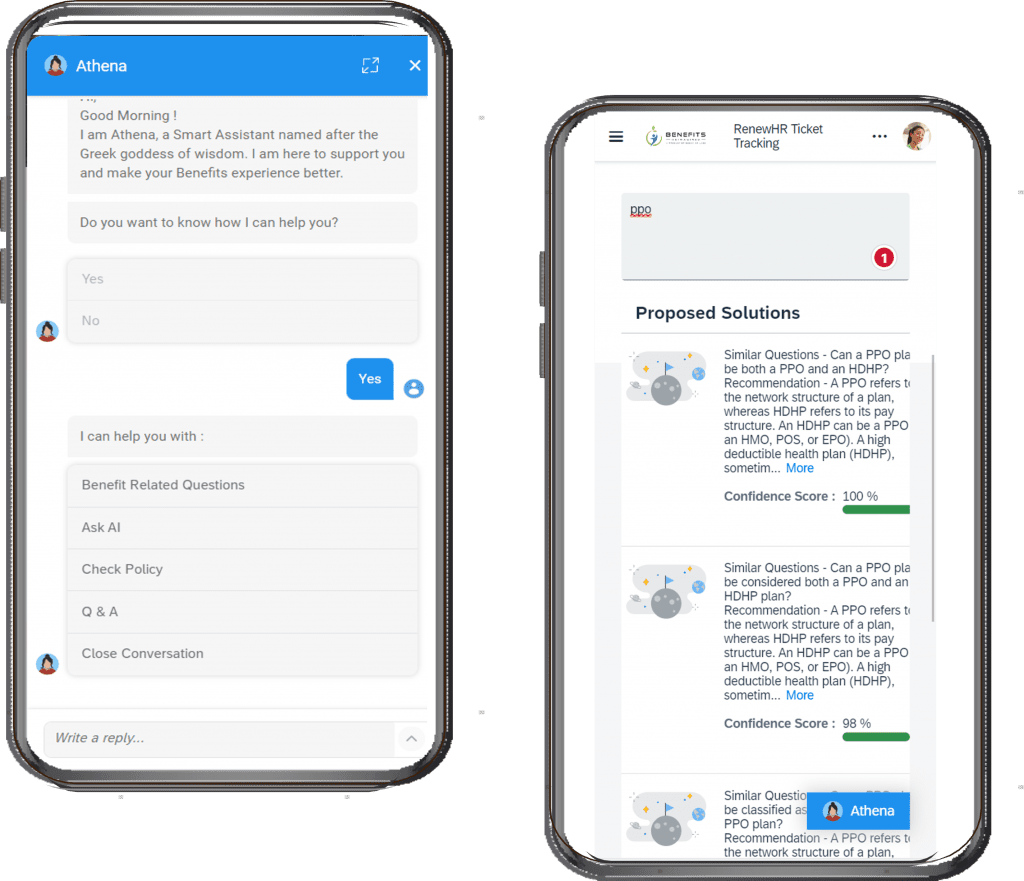
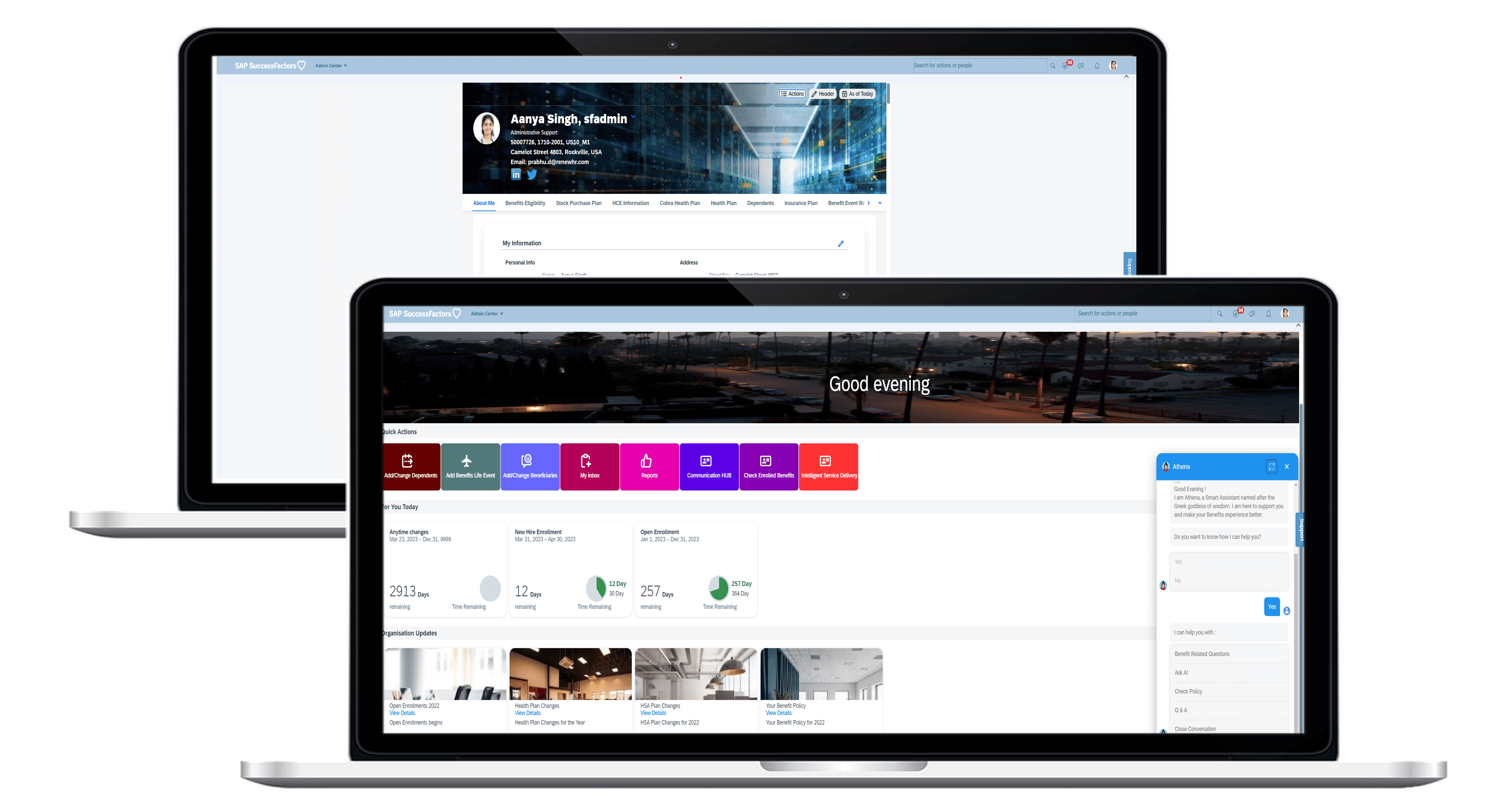
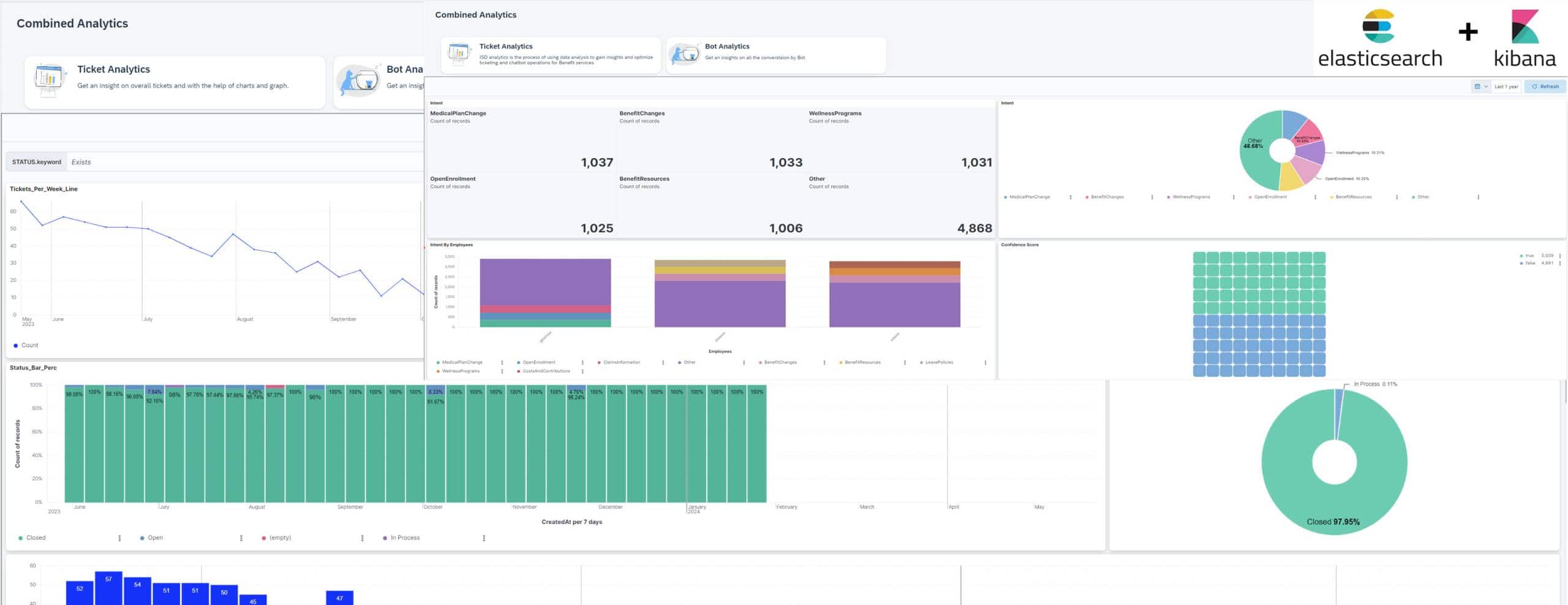
Athena Chatbot
The Benefits Reimagined chatbot, powered by OpenAI and integrated with intent analytics based on Elasticsearch/Kibana, offers several standout features:
Advanced NLP: Leverages OpenAI’s sophisticated NLP for accurate, human-like conversations, enhancing user interaction.
Intent Analytics: Utilizes Elasticsearch and Kibana for real-time intent analysis, improving response relevance and accuracy.
Adaptive Learning: OpenAI employs adaptive learning technology to refine responses based on user interactions, optimizing efficiency over time.
Comprehensive Dashboards: Features detailed Kibana dashboards for visual insights into user interactions and chatbot performance, aiding continuous improvement.
Scalability: Backed by Elasticsearch, it manages high query volumes effectively, ensuring robust performance across enterprise applications.
These features combine to make the Benefits Reimagined chatbot a powerful tool for enhancing user interaction and user intent analytics, making it an integral part of digital Benefits transformation strategies within HR environments.
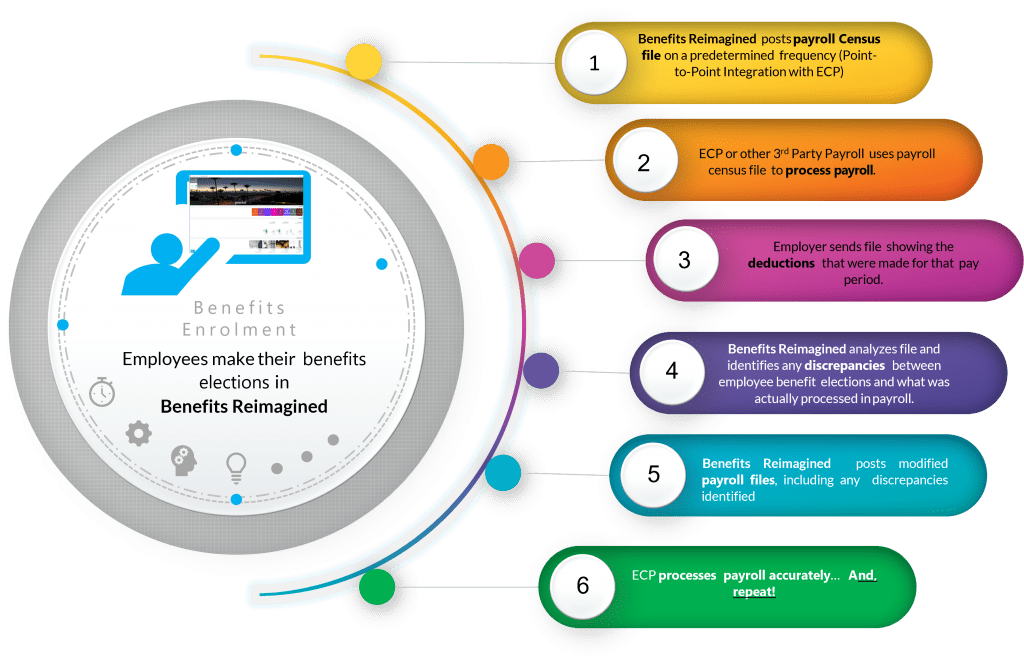
Closed Loop Payroll
- Closed loop payroll or 360-degree payroll, the administrator checks the payroll deduction against the amount the benefits administrator sent on the payroll file.
- This ensures benefits administrator automatically recalibrates deductions with each subsequent payroll file.
- This helps prevent employees from large deductions, the employer and benefits administrator can create company-specific rules per-pay thresholds, and retroactive deductions are automatically prorated.
- An accounting-style payroll billing system that calculates payroll deductions based on the employee’s effective date of coverage and enrollment date.
- Prevent errors in employee benefits expenses.
- Interfaces with the payroll system to import payroll deductions and reconcile, calculating additional deductions and refunds when needed.
- Improve payroll accuracy & benefits process improvement.
- Avoids time spent on manual audits and interventions.
- Calculates retroactive deductions when an employee misses a paycheck because he or she enrolled late or submitted a late-life event.
- Define your payroll schedule, effective date windows, rules for retro deductions, adjustment thresholds, and more.
- Maintain employee confidence & support financial well-being.
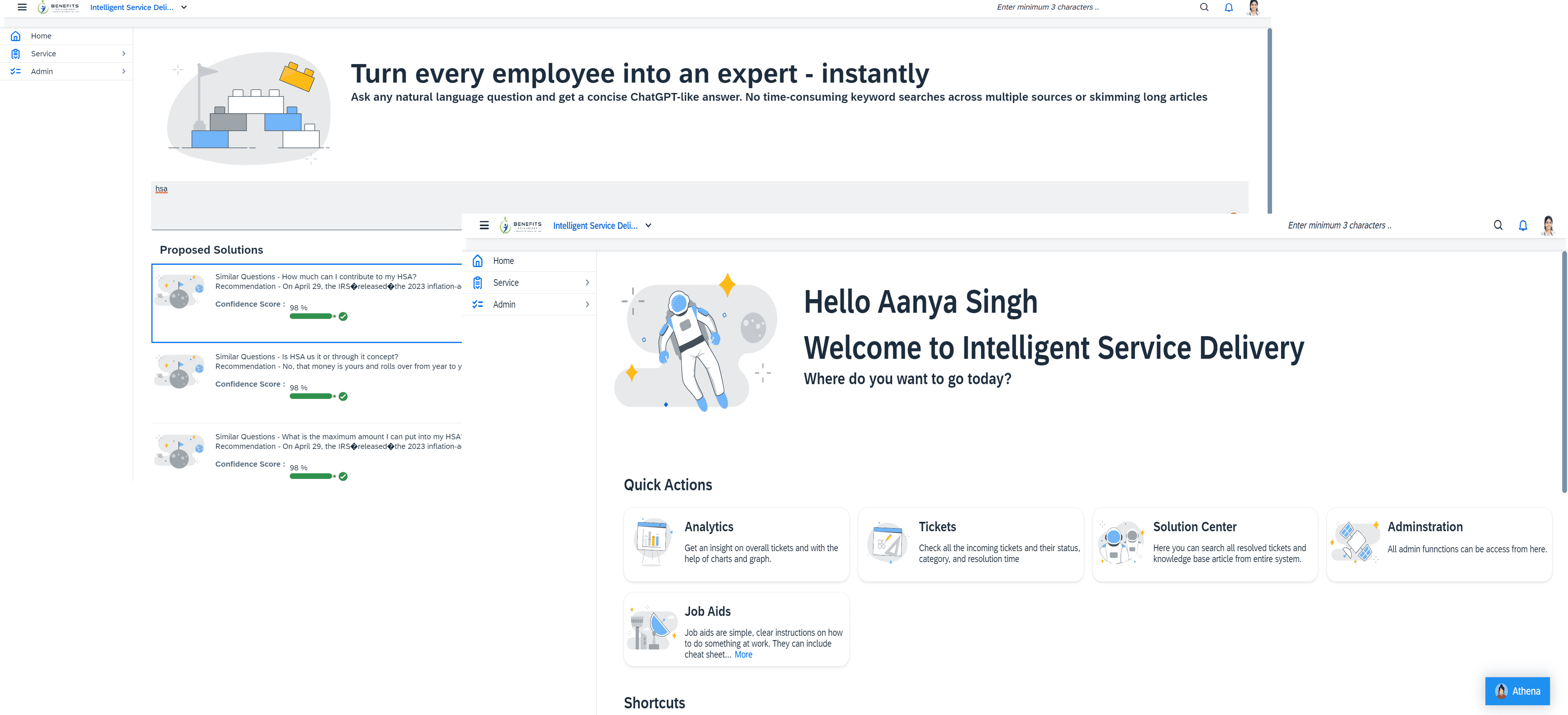
Intelligent Service Delivery (ISD)
Benefits Reimagined’s Intelligent Service Delivery leverages advanced technologies from OpenAI, Elasticsearch, and Kibana to enhance HR operations, offering a scalable, secure, and user-centered experience. Here’s a condensed summary of its core features:
-
- This grounds-up feature combines an AI-driven Chatbot, a ticketing engine, and AI-based answers and sentiment analysis.
- Automation with AI: Utilizes OpenAI’s artificial intelligence for Innovative ticketing and bot-related Analytics to help Benefits administrators understand what employees are looking for and what is effective and work on something that is not working.
- ISD allows customers to bring their email, ticketing, and knowledge management system (KM). We have built it in such a way that we work with what customers are already using for their other enterprise applications.
- Predictive Insights: Integrates Elasticsearch for robust data analytics, providing predictive insights that help benefit administrators anticipate and plan for future needs.
- Personalization: AI is employed to tailor Administrator services to individual administrators’ preferences, enhancing satisfaction and engagement.
- Data-Driven Decisions: Features real-time dashboards powered by Kibana, enabling informed decision-making with visual analytics and key performance metrics.
- Scalability: Designed to seamlessly scale with organizational growth, maintaining performance across varying operational scales.
- Enhanced Security and Compliance: Ensures the protection of sensitive data and adherence to regulatory standards through secure technology frameworks.
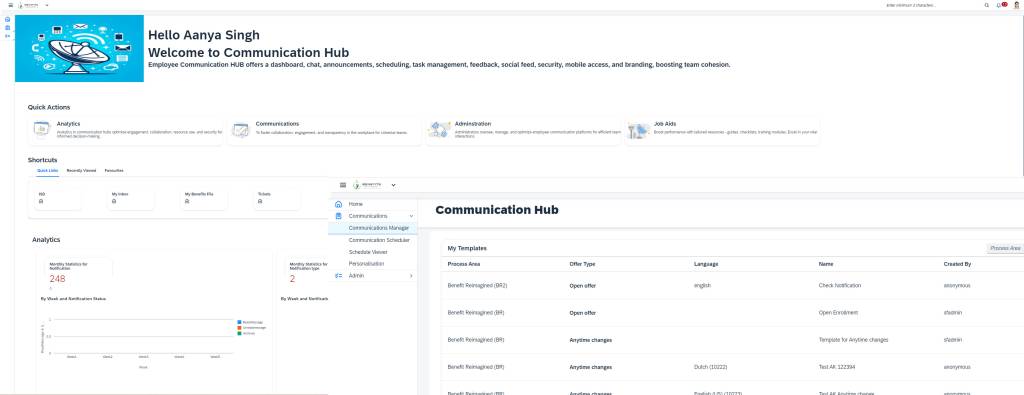
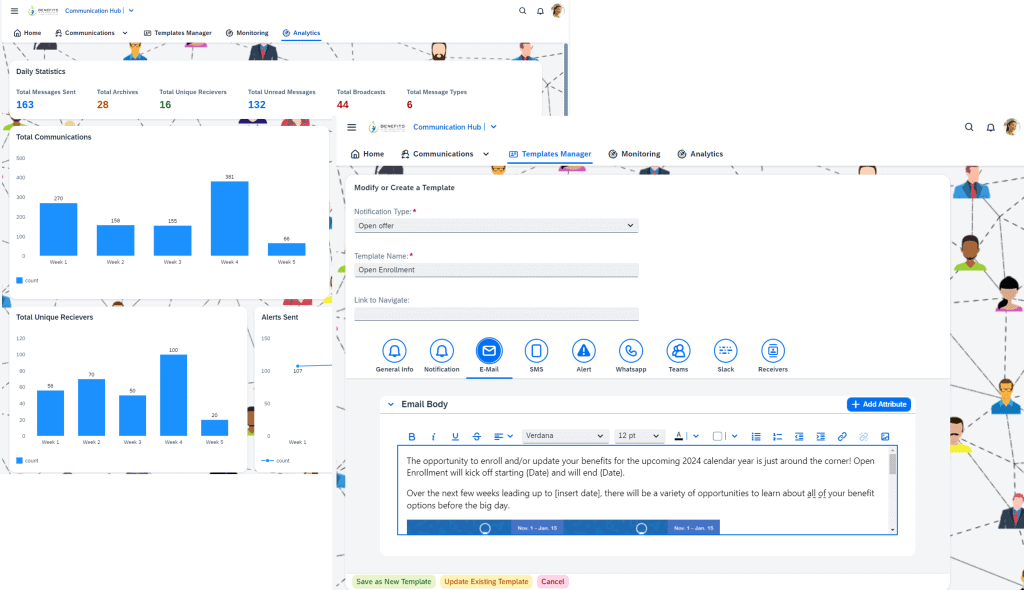
Communication HUB
At Benefits Reimagined, our “Communication Hub” is a centralized solution designed to address the complex challenges Benefits Administrators face in managing employee benefits communication. Recognizing issues such as lack of transparency, inconsistent communication channels, and insufficient clarity for employee inquiries, we have crafted a platform that streamlines these processes effectively.
Key Features of the Communication Hub:
- Centralized Management: All benefits-related communications are administered simultaneously, enhancing control and oversight.
- Customizable Messaging: Tailor communications for different employee groups, such as during “Open Enrollment” periods, ensuring relevance and clarity.
- Diverse Communication Tools: Choose from various channels like email, SMS, Teams, WhatsApp, and more to match the preferred communication styles of different employee demographics.
- Analytics-Driven Insights: Monitor and refine communication strategies with advanced Elastic Search and Kibana-based analytics that track engagement and effectiveness, helping to overcome challenges such as inconsistent messaging and poor onboarding experiences.
The Communication Hub at Benefits Reimagined simplifies the administrative burden by leveraging these capabilities. It elevates the overall communication strategy, ensuring every employee receives timely, clear, and compelling messages tailored to their needs. This approach supports better administrative workflows and fosters a more engaged and well-informed workforce.
Content Management System (CMS)
The Content Management System (CMS) for Benefits Reimagined is designed to enhance Benefits communication and employee engagement through efficient content handling and delivery. Here’s a streamlined overview of its key features:
Centralized Repository: Consolidates all Benefits content in one platform, ensuring easy access and uniform information distribution.
Customization Capabilities: Offers tools for personalizing content to meet diverse employee needs, increasing engagement and relevance.
Automated Processes: Streamlines content workflows with automation, facilitating quicker updates and consistent compliance.
Analytics Integration: Utilizes analytics to monitor content usage and effectiveness, optimizing content strategies.
Benefits Reimagined’s CMS is designed to manage content efficiently and enhance the overall employee experience by providing targeted, engaging, and up-to-date information.
Just like a business, no domain or application can be static.
We are a new solution, but we have big plans for Benefits Reimagined.
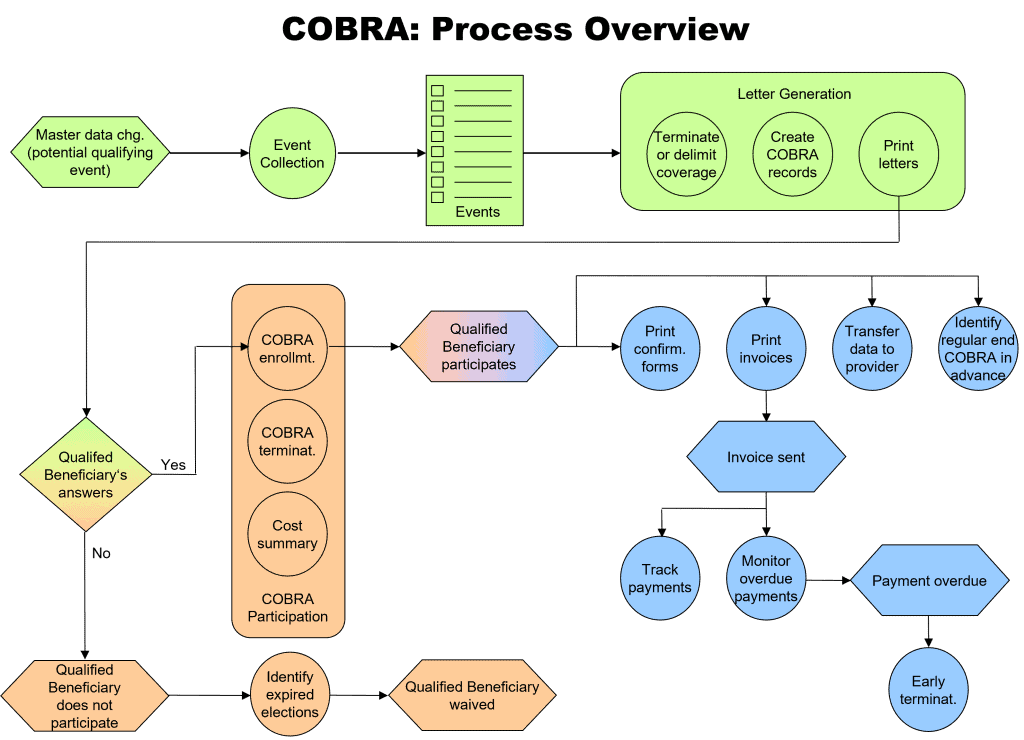
Complete COBRA Process
- COBRA FSA Functionality & COBRA Spending Accounts.
- COBRA events will only consider potential qualified beneficiaries as set up in the system.
- Flexible beneficiary set up.
- Functionality for “Loss of dependent status” based on Age limits, marital or military status, or financial independence.
- Plan Specific “Loss of dependent status.”
- A person can lose his/her dependent status for one plan but not another.
- Can have a loss of dependent status for two different plans on different dates.
- COBRA Letter is restricted to only those health plans and options which a qualified beneficiary was covered under before the COBRA qualifying event.
- Enrolled vs. eligible.
- Health FSA offered on the COBRA enrollment form until the end of the current plan year vs. the end of the COBRA continuation period.
- Ability to include Domestic partners and domestic children as dependents in the COBRA health plan.
- Letter Generation – run batch mode.
- Ability to delete dependents not affected by “Divorce” and “Legal Separation” Events.
- The system creates entries for possible COBRA dependents for all qualified beneficiaries, regardless of whether or not these dependents have COBRA rights of their own (Domestic Partners).
- The system offers health FSAs for enrollment periods overlapping the interval between the loss of regular FSA coverage and the end of the plan year in which the COBRA qualifying event occurred.
- End of FSA Plan Year.
- The system links the updates of COBRA records of additional COBRA-qualified beneficiary types and their possible COBRA dependents when processing COBRA enrollments and terminations.
- Using the COBRA data transfer interface includes health FSA elections of qualified employees and dependents-Transaction.
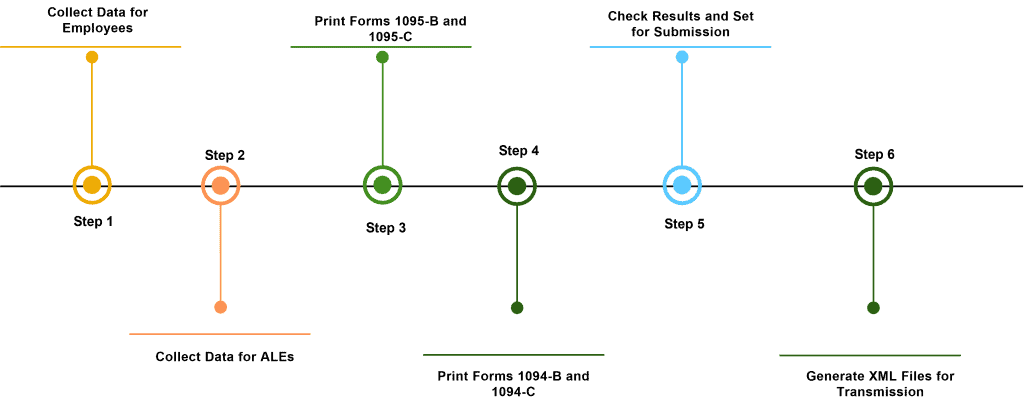
Affordable Care Act Reporting (ACA)
Master Data for ACA Reporting
Before processing employee data for ACA reporting, you must maintain master data in a specific Portlet screen.
Configuring for ACA Reporting
To enable the new functions for ACA reporting, you can make several configuration settings in the system.
Generating Forms
The ACA reporting solution allows you to generate the following forms:
Form 1094-B (Transmittal of Health Coverage Information Returns)
Form 1094-C (Transmittal of Employer-Provided Health Insurance Offer and Coverage Information Returns)
Form 1095-B (Health Coverage)
Form 1095-C (Employer-Provided Health Insurance Offer and Coverage)
Checking Results and Updating Database Records
The ACA reporting solution provides a report that allows checking database data, updating the status of database records, and setting other data for submission.
Database Record Status
The system stores the data of ACA reporting in various database tables, which are updated by the different reports for ACA. For each record, a status is assigned, which indicates the status of the database record within the workflow process.
Submission Status
The IRS submission status enables the system to behave appropriately according to the IRS response to each record. This field is used in the table, which keeps track of the XML files generated for each Run ID.
Advanced Benefits Analytics with Elastic Search & Kibana
The Employee Benefits Analytics from Benefits Reimagined has revitalized and broadened the concept of wellness and employee well-being. It offers employers a framework and valuable data to implement significant organizational changes.
- Advanced Employee Benefits analytics helps you discover where there are any loopholes in your benefits offerings.
- Contribution modeling on benchmarking.
- Comparing your benefit plans and costs to those of your competitors.
- Enhance engagement in your health plan.
- Determine the right strategy for you based on costs and your population.
- Customers can find in-depth analyses of their current and past plan costs, workforce demographics, plan design, or multiple factors.
- Analytics also helps employees and administrators connect with market benchmarking data, which helps in better decision-making.
- The objective is to make every decision and strategy based on what your data is telling you.
Note: APIs for SAC and DWC (seamless integration with Benefits Reimagined) help you bring related data from outside Benefits Reimagined, such as SuccessFactors, Payroll, and many other systems.
The easy-to-use Elastic search and Kibana interface allow developers and Business end users to query data, create catchy charts, and visualize the results via different chart types.
Advantages: Kibana features as an ideal tool:
- For searching, viewing, and visualizing data
- For analyzing the data through charts, tables, histograms, or maps.
- Which has centralized access to built-in solutions developed on Elastic Stack.
- It has dozens of data exploration, visualization, monitoring, and management features.
- Provides dashboard view with all visual elements accessible in any browser.
- Real-time analytical view into large volumes of data.
- As the official interface of Elasticsearch, Kibana is the most effective interface for discovering data insights.
- There is no load on the transactional database.
- Data security applied to index data applies to visualizations as well.
- The seamless interface between the Benefits Reimagined app and Kiban.
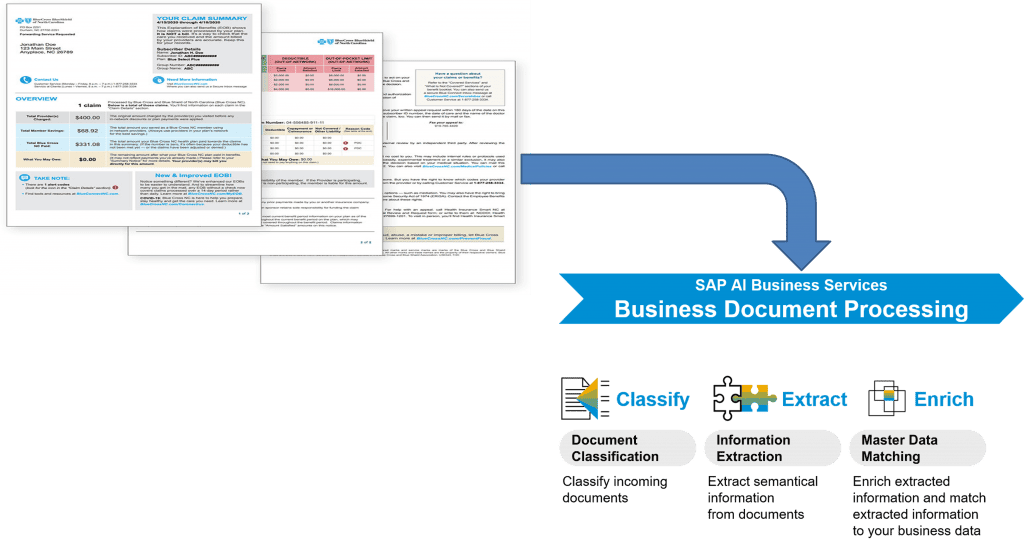
Benefits Reconciliation using AI Services
- Benefit invoice reconciliation is a monthly review of benefits vendor invoices against deductions from your company’s payroll deductions to understand if there are any discrepancies.
- By implementing Invoice Reconciliation processes, companies can achieve significant cost reductions by reducing the need for human labor, increasing automation rate, and higher accuracy by leveraging the latest machine learning algorithms and increasing processing speed and operational efficiency.
- Benefits Reconciliation and Invoice consolidation processing typically consists of the following four steps:
- Classifying: When Vendor invoices arrive, the system understands what type of document it is and decides the next course of action.
- Extracting: Extracts Employee Benefits relevant information.
- Enriching: Extracted information with additional Benefits Data is posted back to Benefits Reimagined for further processing.
- Reconciliation: Benefits Reimagined also extracts Employee deductions from the customer Payroll and can reconcile all three (What is on Benefits Reimagined Enrolled app, vendor invoice, and Payroll deductions) based on custom rules.
Benefits Decision Support System
Benefits Reimagined’s Benefits Decision Support tool is an AI-powered feature that helps employees make benefits decisions by providing personalized recommendations and educational information. This tool considers factors like an employee’s age, job role, family status, salary, healthcare needs, and location to create a list of benefits that are best suited for them.
Decision support systems (DSS) can help businesses in many ways, including:
- Making workflow more efficient: By reducing the time it takes to make crucial decisions, DSS can streamline processes and help businesses accomplish more tasks in a shift.
- Improving planning and management: DSS can help improve planning and increase management success.
- Determining potential outcomes: DSS can help professionals understand the potential effects of their decisions.
- Automating managerial processes: DSS can automate monotonous managerial processes, freeing up managers to spend more time on decision-making.
- Improving interpersonal communication: DSS can improve communication within an organization.
Benefits Reimagined’s DSS can be categorized based on their primary sources of information, including Data-driven DSS, Model-driven DSS, Communication-driven and group DSS, Knowledge-driven DSS, and Document-driven DSS.
Benefits Document Center
Numerous studies have suggested the valuable time an employee spends searching for information, checking for the required documentation, and retrieving already submitted documents inside their benefits Application.
Our DMS solution keeps track of all necessary documentation requirements for the employee. Following are some of the highlights of our solution:
- Offering a one-stop-shop cloud solution to customers. Provides Document Management capabilities on the SAP Business Technology Platform.
- Exposing APIs for consistent consumption for applications through CMIS standard interface.
- Abstracting the complexities of the underlying CMIS-compliant repositories and consistently exposing the features for all the consuming business applications.
- Supporting customer’s Journey by offering connectivity and unified integration to various CMIS compliant Document repository stores, which might consist of Benefits Reimagined, 3rdparty, or SuccessFactors.
- Delivering a ready-to-use embeddable standard unified FIORI User Interface for consistent user experience. This UI would also facilitate the cross-system sharing scenarios.